If you have been experiencing lower back pain (radiating down your leg), numbness, tingling, or weakness for more than a week, or if you are having problems with your bowels or urination physiotherapy for lower back pain could be the solution to your troubles. Below are the causes, and how physio can help decrease your backache.
Quick take: Is physio good for lower back pain?
What Does Physiotherapy do for Back Pain?
For most patients, a month of physiotherapy is enough to relieve lower back pain if there is no underlying condition. Why?
One of the main causes of lower back pain is a sedentary lifestyle. The nature of your work may also contribute to back pain. Think about it; how many hours do you spend hunched over a laptop? Or does your work require you to stand for extended periods?
Physiotherapy for lower back pain is a safe and less aggressive treatment that decreases back pain, improves function and with a good maintenance program, it helps prevent future back pain.
How does physiotherapy work for lower back pain?
Depending on the cause of the pain, you may need active or passive physiotherapy. Active physiotherapy focuses on building muscle strength and repairing the damage. It involves patient specific exercises and stretches.
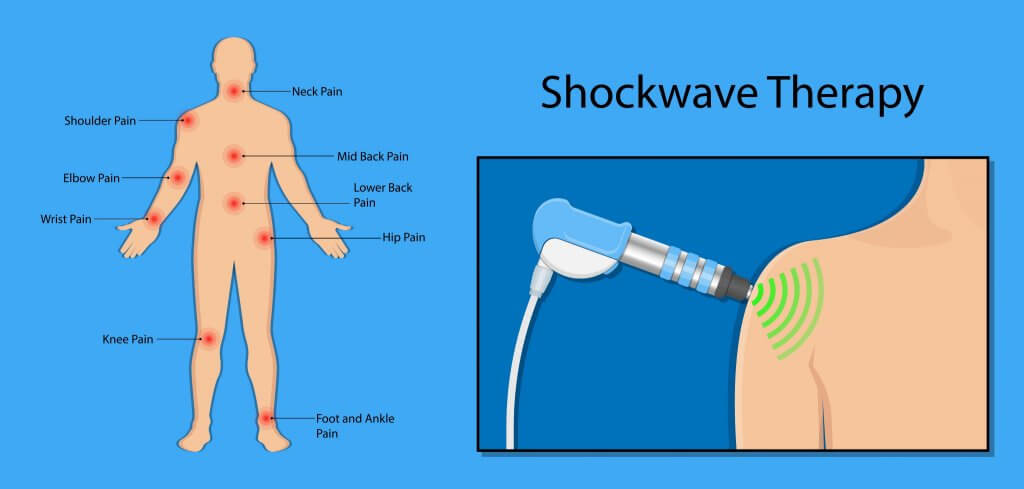
Passive physiotherapy focuses on pain relief. It includes electrical stimulation, heat application, ice packs and patient-specific physical treatments.
Below is everything you need to know about active physiotherapy, including how it can help you recover from back problems and what you can do at home to prevent future flareups.
How do I Know if my Back Ache is Serious?
The Australian Institute of Health and Welfare estimates that between 70 to 90% of people will suffer lower back pain at some point in their lives. The causes include:
- “Spine arthritis” may lead to a condition known as spinal stenosis. Spinal stenosis is the narrowing of the space around the spinal cord that causes lower back pain.
- Osteoporosis is a condition that weakens your bones making them more likely to break. The condition takes several years to develop, and one of its symptoms is lower back pain.
- Muscle and ligament strain. Sudden awkward movements, heavy lifting, and some jobs put you at higher risk of muscle or ligament strain.
- Bulging or ruptured disk. The “disks” in your spine act as cushions, they contain a soft material that may rupture or bulge leading to lower back pain.
Note that the pain may come from your vertebrae, ligaments, discs, nerves, and many other locations in your body. Consequently, you may feel the pain radiate down your leg. For most patients, the pain comes and goes. Meaning you have some good days and some painful ones.
Centralisation of Back Pain: When to see a Physiotherapist
If you experience back pain on and off and it suddenly progresses to your legs, or if you feel the pain developing in other areas of your body, it is time to see a physiotherapist. Also, if you begin exercising and the pain gets progressively worse, your exercise regime could be the cause.
What you need to remember is do not go under any procedure, including x-rays, MRI, surgery, exercise, or take medication before you consult with a physiotherapist. Why?
Pain killers have side effects and only mask the problem, and some patients may have problems such as bulging disks and experience no pain. The best way to understand a patient’s pain is through movement. Experienced Physiotherapists are movement experts who help patients identify the source of their pain and any possible underlying problem.
What to expect when you visit a Physiotherapist with Lower Backpain
- The session will begin with an initial assessment where the physiotherapist will review your medical history and ask you detailed questions about your pain and injury.
- Your physiotherapist will test your range of motion, strength, swelling, nerves, palpation, and ligament and joint stability to diagnose your pain or injury.
- Based on the diagnosis, your physiotherapist will recommend a patient-specific treatment plan.
Physiotherapy Treatment for Lower Back Pain
Depending on the cause of the pain, a physiotherapist will provide you with information on how to manage the pain at home. Treatment may involve
- Manual therapy including massage, joint mobilisation, spinal manipulation, and soft tissue techniques.
- Heat and cold packs.
- Patient specific exercises.
- Dry needling or acupuncture.
- Electrophysical agents such as therapeutic ultrasound, low-level laser, and NMES (Neuromuscular Electrical Stimulation).
How do I strengthen my lower back with physiotherapy?
If you have lower back pain, your physiotherapy treatment plan may include the following exercises. But, before you perform any of the exercises listed below, you should consult with a physiotherapist to avoid further injury or damage to your back:
Core strengthening exercises for lower back pain:
- Wall sits
- Pelvic tilts
- Bridges
- Knee to chest
- Hip stretches
Will Physical Therapy help Arthritis in the Back?
As you get older, the risk of developing arthritis increases. The condition may also result from injury. Some signs that your lower back pain is related to arthritis include, loss of range of motion, weakness or fatigue, nerve pain, stiffness, and back pain.
Physiotherapy helps relieve lower back pain through exercises and stretches that increase flexibility, improve blood flow, and lubricate the joints to improve movement. Physical activity causes weight loss, and that takes some pressure off your joints.
If you have arthritis, your physician may recommend you to a physiotherapist. What a physiotherapist will do is design a treatment program that targets your specific symptoms, the program may include stretching, core building, patient-specific exercises, and aquatic therapy.
Why not do it on your own?
A non-targeted approach may lead to more damage and pain. Consequently, it is in your best interest to work with an experienced physiotherapist.
Will Physiotherapy help Osteoporosis-related Lower Back Pain?
Yes. As mentioned, osteoporosis is a condition that weakens your bones. Physiotherapy helps to strengthen bones, helps manage pain, and prevents bone thinning. If you are above 65, you are at a higher risk of developing osteoporosis.
The condition affects your balance, putting you at higher risk of fall-related injuries.
Through physiotherapy, you can regain your balance and have more energy.
If you have osteoporosis, a physiotherapist will help find suitable weight-bearing exercises aimed at improving your balance and strength. You will also get advice on what to eat, exercises you may do at home and patient-specific advice.
Some signs that your back pain is related to osteoporosis include:
- Brittle bones
- A stooped posture
- Loss of height
- Back pain.
Will Physiotherapy Help Muscle and Ligament Strain-Related Back Pain?
Physiotherapy treatment for muscle or ligament strain may involve dry needling, soft tissue treatment, taping, and load management advice. The treatment varies with the severity of the strain. For example, during the acute inflammatory phase, you may only need hot and cold treatment -whereas, during the repair phase, your physiotherapist may prescribe exercises that help maintain muscle strength and joint range of motion.
What to expect
If you are an athlete or work in an active environment. You are at a higher risk of straining your back muscles. If you go to a physiotherapist, treatment may involve:
- Inflammatory phase: you will get patient-specific advice on how to manage pain, and your physiotherapist may recommend braces or crutches for support.
- Repair phase: to prevent re-injury, your physiotherapist will prescribe exercises to help maintain muscle strength and range of motion.
- Remodelling phase: this stage involves retraining your body’s ability to sense movement, action, and location through exercise.
What are The Benefits of Physiotherapy for Lower Backpain?
To guarantee the best outcome, physiotherapists recommend that you create a full list of all factors that may contribute to pain, including recent injuries, accidents, falls, family medical history, your job, and the sports you play. This will help your physiotherapist to create the most suitable treatment plan.
That said.
Some benefits of physiotherapy for lower back pain include:
Physiotherapy for Lower Back Pain May Eliminate the need for Surgery
As mentioned, before you get surgery or begin taking medication, it is advisable to consult with a physiotherapist. Why?
Physiotherapy may eliminate the need for surgery. On top of that, the recovery window for physiotherapy treatment is shorter than surgery.
Reduces Risk of Injury and Resurgence
Physiotherapy helps to correct underlying issues, including degenerative disease and poor posture, both of which may contribute to lower back pain. Through a structured patient specific treatment plan, a physiotherapist may help you improve your balance, coordination, and strength.
Pain Management Without Painkillers
By correcting your posture, gait, and the way you work or play, physiotherapy can help relieve pain with or without the need for medication. If the pain has progressed or if there is an underlying condition, your physiotherapist may work with an osteopath and chiropractor. Chiropractors specialize in neck and back pain whereas, osteopaths focus on the muscles and joints.
Tip: if you have back pain, you may refer yourself to a physiotherapist. However, in some countries, you may need to be referred by a physician.
Better Mobility
Back pain may lead to stiffness in your back and pain in your legs or other parts of the body. As mentioned, physiotherapists help to pinpoint the root cause of the pain through movement therapy. Once the therapist identifies the cause of your discomfort, treatment will focus on strengthening specific muscles, easing stiffness, and pain management.
Patient-Specific Care
The issue with fixing lower back problems at home is you do not have the training and expertise necessary to tell if there is an underlying condition. Adopting an exercise routine from the internet is problematic in that it may exacerbate the problem leading to more pain.
Why is Physiotherapy/prehab Important Before Lower Back Surgery?
Physiotherapy prepares you for surgery both physically and mentally, and as mentioned, it may eliminate the need for surgery. It also prepares you for life after surgery. You will know what causes pain and how to avoid it through a treatment plan prescribed by a therapist.
Why is Physiotherapy Important after Lower Back Surgery?
Post-surgery, physiotherapy will help strengthen your back muscles, improve your range of motion, and heal tissues damaged by surgery.
If you experience lower back pain symptoms don’t hesitate to give us a call at (02) 9771 1977. Our team at Pro-Fit Physio & Allied Health Centre is always happy to discuss your symptoms and offer the best treatment option.